Throughout Europe, digital innovations with substantial benefits for the patients are spreading quickly. However, stakeholders in Germany are still reserved about these new technologies. Alexander Schachinger, founder and CEO of healthcare42.com and speaker at Health 2.0 Europe, talks about the chances of digital healthcare services in Germany.
30 October 2012, questions by Martin Schmucker
Mr. Schachinger, healthcare42 and Publicis Healthware / razorfish are currently preparing a survey about the utilization of health information by chronic patients in the Internet. What exactly is the objective of your investigations?

Alexander Schachinger: Up to now, there haven‘t been any representative scientific studies about the usage of health information by chronic patients. We still don‘t know how this influences their knowledge, their attitudes or their behavior in regard to the healthcare market, in particular towards doctors and pharmacists. We are attempting to close a gap here since research on e-patients has been unfortunately neglected in Germany. In a survey in cooperation with KWHC and others, we interviewed 3,500 e-patients online. We were able to show that the internet, exchange in forums and suchlike do have an effect on the patients, especially in regard to medical consultations and the decision for or against a certain therapy.
How do you define “e-patients”?
With this term we refer to people suffering from chronic diseases, but also to acutely ill patients, who use the Internet to find out and share information about health issues. This term also comprises all sorts of caregivers, including parents, children or spouses who inform themselves about the medical conditions of their loved ones via the Internet.
What information are e-patients usually searching for?
They are searching for explanations for their symptoms, but also for information about therapies, treatments and drugs. E-patients also search for recommendations and evaluations of hospitals and doctors. Sharing information with their fellow sufferers in forums such as med1.de, imedo.de or netdoktor.de is regarded as very valuable by chronic patients – we call this the “patients like me” approach. Another important result of our first survey is that e-patients are very critical. They challenge their doctors‘ diagnoses and search for alternatives to the therapies suggested by their physicians.
The information found in forums often originates from non-professionals. Isn‘t there a fundamental conflict with professionally validated information? How can the quality of the information be assured?
My answer here may be somewhat provocative: this question derives from a very traditional mindset in the healthcare sector in which the doctor appears as the sole keeper of medical knowledge. Issues like quality assurance and data protection are often perceived as threats – a typical reaction and a typical attitude in the German healthcare system. Non-traditional players on the market produce the major part of health communication in the Internet. In terms of audience reach, it‘s the publishing houses and the start-ups that are in charge of leading health portals and communities. Patient-generated information does not at all challenge evidence-based medicine or treatments prescribed by physicians. Rather than that, both complement each other since the traditional players in healthcare don‘t succeed in providing relevant content for chronic patients and their practical, every-day problems. There is often a lack of understanding for the chronic patients‘ every-day perspective. Some improvements could certainly be reached by means of targeted trainings in patient information for doctors.
What are the causes for the lack of understanding of the patients‘ perspective?
There is a discrepancy between supply and demand. Patients want hands-on help for their every-day problems. If the physicians don‘t provide this, the patients start helping themselves. Similar patients with similar problems speak the same language and look for similar solutions. In network research, we call this “communities of practice”. But there is also a structural problem: physicians are bound to many regulations and to the framework of health economics. Not least the “red tape” is to blame that the time to talk with their patients is very limited: they have five minutes per patient and per quarter. However, a diabetes patient is sick 24/7. In a forum, he can ask his questions anytime, from anywhere. We found out: on average, questions posted in forums are answered by seven other patients and after only 17 hours. These values are phenomenal and could by no chance be reached in a face-to-face interaction between doctors and patients.
In your opinion: what are the most important developments in the field of digital health? Which applications and software solutions are trendsetters in the future?
With the beginning of the Health 2.0 Europe conference, we will publish an analysis of the 800 most visited healthcare websites. Without a doubt, the non-traditional players, i.e. start-ups and publishing houses, reach the largest audiences and are most up to date. Among them there are numerous services that support therapy and offer real benefits to the patients: search and exchange functionalities on websites, mobile services for particular conditions, patient-generated feedbacks evaluating the outcomes of therapies, and many others. Hospitals and health insurances have developed rather moderate-sized pilot projects. In Germany, we still have a long way to go until we really manage to connect the traditional players‘ health services with digital services.
Why are the traditional players lagging so far behind?
Perhaps a comparison will help: in the Middle Ages, monks used to demonize the printing press. Not so long ago, Microsoft‘s managers used to refer to Open Source and Linux as “communism“. The same attitude towards innovation often occurs in the ambit of healthcare: according to a widespread opinion, there is no quality to be found in Internet services. Also, the motivational structures are critical: the health insurances‘ schedules of benefits don‘t cover digital services. Health-related apps or patient communities in which those affected exchange how they cope with a disease are not being paid, although it is a matter of fact that they can positively impact knowledge and compliance. Clinics and pharma companies have no economic incentives to invest. For start-ups, this means that they must finance themselves via advertising or let the patient pay for their services.
Can you name exemplary innovations?
We present the research project on our website. At Health 2.0 Europe, I will give a first overview. We will publish a press release on our first systematic online market analysis in a couple of days.
What awaits us in your panel at the Health 2.0 Europe conference?
I will give an introduction into the digital activities of pharma companies worldwide and in Germany. Digital innovations can significantly contribute to improving patient care and medical research. On top of that, we are currently witnessing a fundamental change in the business models of the pharma industry. There are some first approaches how these companies can evolve from drug sellers to providers of all-embracing health services beyond the medicine. In my lecture I will address recent developments and medium-term scenarios.
Do digital innovations offer chances to reduce costs in healthcare?
The potential is enormous. The non-compliance costs are estimated to about 30 billion euros in Germany alone. Tailor-made digital services for medical assistance, education and patient feedback can contribute to optimizing healthcare, cutting costs and at the same time facilitating evaluation of different treatments from the every-day perspective of the patients. This approach is called “information therapy“ – providing the right information to the right patient at the right time.
Let‘s have a look at the bigger picture: where is Germany in the field of digital health, compared to other countries?
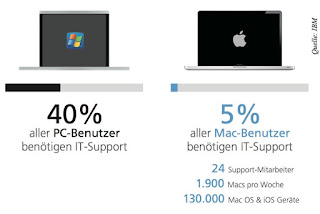
Smaller countries, especially in Europe, are far ahead of Germany. In Denmark, digital healthcare services have already been implemented on a national scale. In Switzerland, the planning is well advanced. In these countries, electronic health records are available to everyone. Patients can check their X-ray images, physicians‘ letters, and other data online. In the Netherlands, we see an exemplary cooperation and pilot projects between hospitals, universities and patient platforms. There is a real online communication between patients and physicians. There is no reason why this shouldn‘t also be implemented in Germany. Online services hold a huge potential in terms of market positioning, especially for hospitals that are in harsh competition. Sadly, the diagnosis so far is: there is a widespread ignorance among traditional players regarding issues of digital healthcare, although about 40 million Germans search the internet for health-related information on a regular basis. I suppose that the country cannot afford this for much longer.
###
About Health 2.0 Europe
Health 2.0 Europe is the premier conference dedicated to how Web 2.0 and social media are transforming healthcare systems in Europe. The conference brings together professionals in the converging industries of healthcare, the internet, mobile applications and social media to address how Web 2.0 and mobile technologies revolutionize both healthcare delivery and treatment. Health 2.0 Europe is organized by pioneering experts with decades of combined experience in health- and web-related business and consulting, including Matthew Holt and Indu Subaiya, founders of Health 2.0 in San Francisco. Please visit www.health2con.com/europe for more information, or follow Health 2.0 Europe and its online communities and groups on Twitter, LinkedIn and Facebook.
About Alexander Schachinger
Alexander Schachinger is a self-confessed Health 2.0 addict. Following a career in digital media consulting in Germany and Canada, he is now both completing a Ph.D. At Health 2.0 Europe he will share his research results of the first qualitative e-patient online survey and health web site analyses on a national scale ever done in Europe.

 Kundenbindung stärken und die pharmazeutische Beratung unterstützen: Das sollen Apps leisten, die Apothekenkunden in der Regel kostenlos nutzen können. Die deutschsprachigen und kostenlosen Apotheken-Apps wurden im Dezember 2013 von der Initiative Präventionspartner geprüft. Welche Servicefunktionen bieten diese Apps, wie gut schneiden sie im Hinblick auf die Qualität und Transparenz der gesundheitsbezogenen Informationen ab (HealthonApp-Ehrenkodex)? Sehen […]
Kundenbindung stärken und die pharmazeutische Beratung unterstützen: Das sollen Apps leisten, die Apothekenkunden in der Regel kostenlos nutzen können. Die deutschsprachigen und kostenlosen Apotheken-Apps wurden im Dezember 2013 von der Initiative Präventionspartner geprüft. Welche Servicefunktionen bieten diese Apps, wie gut schneiden sie im Hinblick auf die Qualität und Transparenz der gesundheitsbezogenen Informationen ab (HealthonApp-Ehrenkodex)? Sehen […]